Chair's Column: The Experience of a Lifetime
Dr. Gillian Hawker
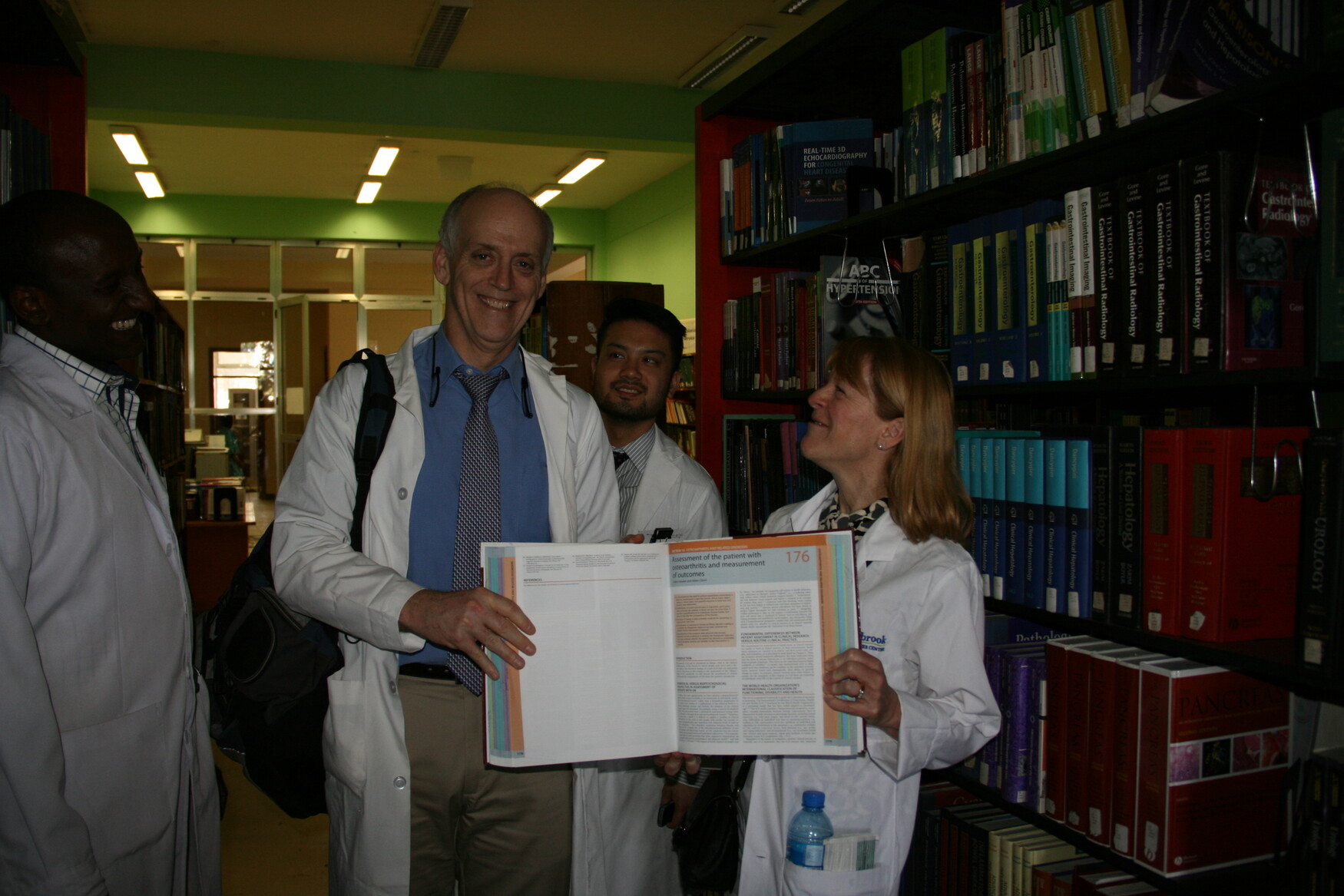
A few weeks ago, I had the experience of a lifetime – I accompanied two of our hematology faculty members – Gena Piliotis and Michael Crump, along with hematology PGY5 trainee, Eric Tseng, to Addis Ababa to see for myself what our colleagues have been doing to train specialists in Ethiopia. I knew about TAAAC – the Toronto Addis Ababa Academic Collaboration – but I didn’t really have a good sense of what it was all about, or how it differed, if at all, from the many other global outreach initiatives with which our faculty are engaged.
We set off as a group on March 12th – Drs. Crump and Tseng were going for a month (the prerequisite time for faculty/residents who wish to volunteer) and Dr. Piliotis was my field guide and chaperone – she was going to ensure I ‘got it’ by the end of my visit. And, no surprise, I did. I am writing now to tell you about this first experience with TAAAC and to get your input on where we should go next, as a department, with this initiative.
As described elsewhere in this newsletter, TAAAC represents a partnership between U of T and Addis Ababa University designed to increase capacity for healthcare in Ethiopia, which has a population of approximately 90 million. When TAAAC first started, primary care and emergency medicine did not exist; individuals with mental health issues were locked away, and there were few internal medicine specialists. Since then, we have visited regularly, one month at a time, to provide faculty oversight in residency training in the subspecialties of internal medicine – not to deliver care ourselves, but to work alongside the resident trainees to translate their book knowledge to clinical practice. With few exceptions, we don’t bring the Ethiopian trainees to U of T; the stats show that if we do, the chances that they will return to Ethiopia, where they are desperately needed, are reduced.
To date, members of our faculty – and a number of senior residents - from the Divisions of Hematology, Endocrinology, Emergency Medicine, Gastroenterology, and Nephrology have spent time in Addis. In this edition of the newsletter, you will hear from two such residents – Emilie Chan, PGY6 in nephrology and Eric Tseng, PGY 5 in hematology. We also asked Dr. Piliotis – our TAAAC ringleader, to give us the history of TAAAC, its accomplishments, and what is needed to sustain and build TAAAC. But first, I’d like to provide you with a few reflections of my own on my first – and hopefully not last – trip with TAAAC.
This is what I learned:
TAAAC is all about building capacity for health and healthcare through the training of physicians. To my knowledge, this distinguishes TAAAC from the many, many other global and local outreach initiatives in which we are engaged, which are largely focused on either research/advancing new knowledge or providing care directly (e.g. Médecins Sa ns Frontières).

‘Dr. Gena’ is revered and adored at AAU and the Black Lion Hospital, where the Ethiopian residents train and our faculty/trainees educate. Everyone – from the fellow at the gate to the hospital nurses, physicians, even patients, knew ‘Dr. Gena’ and greeted her with delight. Clearly, Dr. Piliotis has been a superb ambassador for our department and deserves our thanks. She is also an amazing teacher – watching her interact with the residents was a definite highlight of my trip!
What TAAAC does is unique. I heard time and again from the senior AAU faculty members how incredibly valuable it is for our faculty/senior residents to come and stay put for a month. Other universities show up regularly, but only U of T devotes sufficient time at the side of the AAU trainees in clinic, on the wards, and examining slides or images, to make a difference to their education. They are very grateful.
The AAU residents are super bright, clearly committed to their training and a pleasure to spend time with and teach – even after hours and hours of time with our faculty, they are asking for more. It is a great pleasure to be there, where your ideas and suggestions are so valued and respected.

The patients seen in clinic and on the wards were really sick – I saw pathology that I have never seen before, including in a rheumatology clinic. (There are no rheumatologists but the medicine residents run a clinic anyhow.) The diagnostic dilemmas were intellectually stimulating. It was an incredible opportunity to use ALL of my internal medicine training and knowledge.
The country is poor with few resources – access to tests, medications, procedures, etc. is highly variable – there was not one consultation I recall where the social health determinants did not factor into our clinical decision making. The hospital is old and past due for a renovation, with paint and plaster coming off the walls and ceilings and no potable running water in many parts of the hospital.
Life is expendable. The median life span for Ethiopians is in the mid-fifties. If you get to be ‘aged’ you’re fortunate. Life and death decisions occur every day, many times a day – can we provide chemotherapy to this patient? The patient with acute renal failure who cannot afford to go to India for a renal transplant will die. The patient who lives hundreds of miles from Addis will not be able to receive the necessary weekly or monthly therapy.
Learning goes both ways. I learned a lot about innovative ways of teaching from my visit. Not that we would or should duplicate the regular practice of four residents each seeing their own roster of patients in a single exam room (with one exam bed and no curtains for privacy), but there were some really important benefits to this scenario. First, the faculty member in that room with the trainees was providing direct supervision to all the trainees (not running their own clinic alongside). Whenever one of the residents had a question or needed some advice, the faculty member was right there and, often, the other residents would stop to listen and learn as a group. The patients were clearly so grateful for the care they were receiving that no one complained about the wait. Is this competency-based training in action? Second, the clinic ran chaotically, but efficiently – hundreds of patients were seen by the team of residents in any one half day. Nurses and clinic assistants moved charts around as the residents completed their consults and follow-up visits to ensure all patients were seen by the next available resident – they pitched in when one of their colleagues had a difficult/complicated case that required more time. A wonderful example of patient-centred team based care!
As one of our faculty members said more eloquently than could I:
“What I learned from the trip, I worry, is more than I gave to the cause. I learned the art of the physical exam once more and of the broad differential diagnosis in medicine, particularly when in an under-resourced and tropical area. I was reminded of the importance of patient advocacy and judicial use of resources that either the person or the system cannot entirely afford, or the patient travels 800km to come to follow up clinic. I learned about the challenges of embarking on treatment when there is no support for its complications.”
So, what does the future hold for TAAAC?
As Dr. Piliotis states in her editorial, TAAAC has been a huge success with tangible benefits to the lives of Ethiopians as well as to those faculty and trainees who have participated. As a result, TAAAC is hoping to expand to include training programs in additional specialties within medicine. But there are a number of barriers that must be addressed. A month spent away from Toronto has implications not only for clinical care (‘on call’ and daytime work) and income (personal and practice plan), but also to one’s family (wait till kids have flown the coop to go to Addis?) These are serious challenges that, to date, have not been systematically addressed at the departmental or faculty level. Perhaps it’s time now?
So I would like to hear from you – what should we do about TAAAC?
We could choose to leave TAAAC as it is – an initiative reliant on volunteers. Alternatively, as the largest Department of Medicine in Canada, we could take some ownership of TAAAC. IF we agreed that TAAAC is a good thing and should be supported, we might consider the following:
1. Establish a competitive resident elective where senior residents would apply to spend one month in Addis (in the final six months of their training), contingent on identifying a willing U of T faculty member to take along. We would cover the resident’s expenses and provide a reasonable stipend to the faculty member. We would work with advancement to raise the necessary funds.
2. Given our research strengths, we could use these visits to leverage research initiatives. Leaders at AAU want to build their academic capacity in basic and clinical research. We could formalize a research partnership with AAU to advance collective research priorities, e.g. partnering with AAU to train/supervise clinician-scientists focused on tropical diseases, TB, autoimmune diseases, nutritional deficiencies, etc. We might identify potential trainees through our educational outreach.
Please email, tweet, telephone, or use whatever medium you prefer to let me know what you think. Thanks in advance.